Understanding Inflammation Of The Upper Female Reproductive Tract
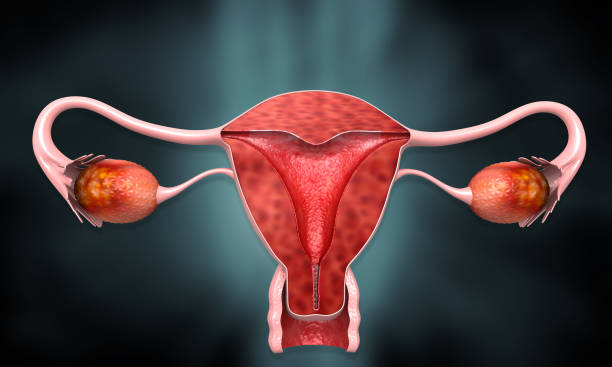
Pelvic Inflammatory Disease (PID), a complex and often under-recognised condition, represents one of the most consequential forms of inflammatory disorder affecting the upper female reproductive tract. Involving critical anatomical structures such as the uterus, fallopian tubes, and ovaries, PID is frequently the sequela of sexually transmitted infections— most notably Chlamydia trachomatis and Neisseria gonorrhoeae—as well as bacterial vaginosis and invasive gynaecologic procedures that breach the cervical barrier.
Among its clinical presentations, salpingitis— characterised by inflammation of the fallopian tubes—emerges as the most prevalent and diagnostically significant form. Yet, despite its ubiquity in clinical practice, PID is often underestimated in terms of its long-term impact on reproductive health, including chronic pelvic pain, ectopic pregnancy, and infertility.
It is fundamentally a preventable condition.
Pelvic inflammatory disease is, essentially, caused by the body overreacting to an infection. As the immune system tries to fight off the invading bacteria, it causes local inflammation and scarring. Although this may successfully wall off the infection inside the reproductive tract, it can damage the organs. PID can cause scarring in the uterus, fallopian tubes, and even in the pelvic cavity. This is one of the main reasons it causes chronic pelvic pain.
The most common infections associated with pelvic inflammatory disease are chlamydia and gonorrhea. Because the symptoms of PID are the result of the body’s response to the underlying infection, treatment usually involves antibiotics to treat that infection. In severe cases, or an emergency, surgery may be necessary to drain an abscess that has ruptured or threatens to rupture.
Symptoms
®Pain in the lower abdomen and pelvis
®Irregular periods
®Pain during sex
®Pain during urination
®Lower back pain
®Excess vaginal discharge with a foul odour
®Fever, exhaustion, diarrhea, vomiting, and other general signs of infection.
Is PID common?
In the early 1990s, the self-reported frequency of PID in women was approximately one in nine. PID was more than twice as common in women with a history of sexually transmitted diseases (26 percent) than among women who had never reported an STD (10 percent).
Risk factors
Younger age: Sexually experienced teenagers are three times more likely to be diagnosed with PID than their 25- to 29-year-old counterparts. Scientists do not know, however, whether this is due to biological factors that make young women more susceptible to STDs or different sexual behaviors in these two age groups.
Women have the highest risk of PID of the ethnic groups seen in the U.S. This may be related to biological factors, or due to their comparatively high frequency of douching.
Contraceptive Choice: Barrier methods, such as condoms, and oral contraceptives reduce the risk of PID.
Douching: Douching greatly increases a woman’s risk of PID.
Concerns about PID
Worldwide, PID is one of the leading causes of ectopic pregnancy and preventable infertility in women.
Pelvic inflammatory disease can cause infertility by damaging the fallopian tubes. This damage can block the tubes, making it difficult for a fertilised egg to reach the uterus.
What duration does it take to become infertile with PID?
PID can permanently scar and damage the fallopian tubes, causing blockage of the tubes. About 12 percent of women suffer enough tubal damage from one episode of PID to become infertile. After three episodes of PID, the infertility rate reaches 50 percent.
It is less expensive to prevent PID-related infertility than to treat the STDs and PID that cause infertility and resolve infertility in couples who wish to become pregnant. Ultimately, the costs of preventing PID-related infertility are probably much lower. Those costs would primarily include those for education about safer sex, douching, and condom use as well as screening and treatment for chlamydia and other STDs. Such preventive measures would probably be only a small fraction of the cost spent on treatment.
The relationship between PID and infertility is relatively well-accepted. PID causes infertility by the scarring process that occurs during the healing of sexually transmitted infections. The extensive scarring can eventually occlude one or both fallopian tubes, and scarring tends to be worse among older women, smokers, and women using IUDs. Depending on the extent of scarring it may be impossible for sperm to reach the egg, or, if sperm can get through, the fertilised egg may be unable to get to the uterus.
Not surprisingly, the percentage of women who experience infertility due to PID is directly proportional to the number of episodes of PID that they have experienced. Therefore, both treating and preventing PID are important steps in the reduction of infertility.
Dr Taiwo Orebamjo is an experienced Consultant Obstetrician and a medical administration expert from the Kingston Academy of Learning and Career College Canada. He is a post-graduate of the Royal College of Obstetricians and Gynaecologists, London. The Research Fellow in assisted conception at the St. George’s Teaching Hospital in Tooting London is also the Consultant Obstetrician &Gynaecologist, Medical Director, at Parklande Specialist Hospital & Lifeshore Fertility and IVF Clinic.
